8 types of diabetes: Causes, symptoms and treatment
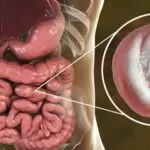
The 8 types of diabetes encompass a variety of conditions, with the most widely recognized being Type 1 diabetes, Type 2 diabetes, and gestational diabetes mellitus.
These particular forms are primarily associated with either reduced insulin production by the pancreas or the body’s inability to effectively respond to insulin, a condition known as insulin resistance. Both scenarios lead to elevated blood sugar levels and, if unmanaged, can result in serious health complications.
In addition to these, there are several less commonly known types of diabetes that fall within the broader classification.
These include diabetes insipidus, which, despite sharing the name, is a distinct condition that does not involve blood sugar regulation; latent autoimmune diabetes in adults (LADA), which exhibits traits of both Type 1 and Type 2 diabetes but develops later in adulthood; and maturity-onset diabetes of the young (MODY), a rare, inherited form of diabetes that also presents characteristics of both primary types.
Determining the specific type of diabetes a person has is a critical step toward effective management and is typically carried out by a healthcare professional, such as an endocrinologist or a primary care physician.
These specialists will conduct appropriate diagnostic tests and evaluations to identify the exact form of diabetes. Once diagnosed, the treatment plan is tailored to the individual’s needs and may involve a combination of nutritional adjustments, physical activity, oral diabetes medications, or in some cases, insulin therapy to help control blood glucose levels and prevent complications.
8 types of diabetes
The primary classifications among the 8 types of diabetes include the two most widely recognized forms: Type 1 diabetes and Type 2 diabetes. These are considered the major forms due to their prevalence and long-term impact on global health.
- Type 1 Diabetes
Type 1 diabetes is a relatively less common but serious autoimmune form of diabetes in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells of the pancreas. As a result, the pancreas either produces very little or no insulin at all, leading to abnormally high glucose levels in the bloodstream.
This form of diabetes often develops at a young age, commonly during childhood or adolescence, and tends to present with sudden and noticeable symptoms. Individuals may experience frequent urination (polyuria), unquenchable thirst (polydipsia), increased appetite (polyphagia), and unexplained weight loss, all of which are hallmark signs of elevated blood sugar levels.
Management of Type 1 diabetes requires a lifelong commitment to insulin therapy, since the body can no longer produce insulin naturally.
Treatment usually involves daily insulin injections or the use of an insulin pump to regulate blood glucose levels and prevent acute complications such as diabetic ketoacidosis. This type is one of the more serious entries within the 8 types of diabetes and demands constant monitoring and lifestyle adjustments.
- Type 2 Diabetes
Type 2 diabetes stands as the most widespread and prevalent form within the 8 types of diabetes. It is primarily marked by insulin resistance, meaning the body’s cells no longer respond efficiently to insulin. In some cases, there is also insufficient insulin production, making it difficult for the body to maintain stable blood glucose levels.
This type is more commonly diagnosed in adults over the age of 40, though it is increasingly seen in younger individuals, including children and adolescents, particularly due to rising obesity rates and increasingly sedentary lifestyles. Genetic predisposition plays a significant role, but environmental and lifestyle factors such as physical inactivity, poor diet, and excess body weight are major contributors.
In the early stages, Type 2 diabetes may be asymptomatic, making regular screening vital for early detection. When symptoms do occur, they may include dry mouth, excessive thirst, blurry vision, slow-healing wounds, and fatigue—all resulting from prolonged high blood sugar levels.
Treatment for Type 2 diabetes typically begins with lifestyle modifications. These include adopting a balanced diet, engaging in regular physical activity, and working toward healthy weight loss.
If lifestyle changes alone are insufficient, physicians may prescribe oral antidiabetic medications such as metformin, gliclazide, semaglutide, or dapagliflozin. In more advanced cases or when blood glucose remains uncontrolled, insulin therapy may also become necessary to manage the condition effectively.
- Type 3 Diabetes
Type 3 diabetes is a proposed form of diabetes that has gained attention in recent years due to its suspected connection between insulin resistance and cognitive decline, particularly in individuals affected by Alzheimer’s disease.
Although it is not yet formally recognized as an official medical diagnosis by the global medical community, growing research suggests a potential link between brain insulin dysfunction and neurodegenerative disorders.
In this context, Type 3 diabetes is believed to occur when the brain becomes unable to respond properly to insulin, much like what happens in peripheral tissues in other forms of diabetes. This insulin resistance in the brain may impair memory and learning functions, leading researchers to explore its possible role in the development and progression of Alzheimer’s disease.
Despite its controversial classification, some researchers and health professionals consider Type 3 diabetes an emerging area of study within the broader scope of the 8 types of diabetes, particularly because of its implications for aging populations and neurological health.
- Gestational Diabetes
Gestational diabetes is a unique form of diabetes that arises specifically during pregnancy, typically around or after the 24th week of gestation. It is characterized by a temporary disruption in insulin production and function, resulting in elevated blood sugar levels that can affect both the mother and the developing baby.
This condition is part of the 8 types of diabetes and is usually diagnosed for the first time during routine prenatal screenings, even in women with no prior history of diabetes. While the exact cause is not always clear, gestational diabetes is often associated with hormonal changes during pregnancy that interfere with the body’s ability to use insulin effectively.
Certain risk factors increase the likelihood of developing this type of diabetes, including a family history of diabetes, being overweight, advanced maternal age, or following a diet high in processed sugars and unhealthy fats. Women who lead inactive lifestyles before or during pregnancy may also face a higher risk.
The symptoms of gestational diabetes often mirror those of Type 2 diabetes and may include excessive thirst, increased urination, fatigue, and blurred vision. In many cases, however, the condition is asymptomatic and only discovered through routine glucose testing.
Treatment usually begins with dietary modifications focused on low-glycemic foods and regular exercise to improve insulin sensitivity. If lifestyle adjustments are not sufficient to maintain healthy blood sugar levels, medications such as insulin may be prescribed to protect both maternal and fetal health.
Fortunately, this form of diabetes usually resolves after childbirth, although women who have experienced gestational diabetes are at a greater risk of developing Type 2 diabetes later in life. Continuous postpartum monitoring and lifestyle adjustments can significantly reduce this risk.
- Maturity-Onset Diabetes of the Young (MODY)
Maturity-onset diabetes of the young (MODY) is a rare and inherited form of diabetes that typically emerges during adolescence or early adulthood. Unlike Type 1 diabetes, which is autoimmune in nature, or Type 2 diabetes, which is often linked to lifestyle, MODY is caused by a mutation in a single gene and is passed from parent to child. This makes it a monogenic type of diabetes and a notable entry among the 8 types of diabetes.
MODY tends to develop in individuals under the age of 25, and its presentation is generally milder than that of Type 1 diabetes. In many cases, it can even go undiagnosed for a period due to its gradual onset and less severe symptoms.
When symptoms do appear, they may include excessive thirst, frequent urination, recurrent infections, or elevated blood glucose levels detected during routine testing.
What sets MODY apart from other types within the 8 types of diabetes is that it shares some traits with both Type 1 and Type 2 diabetes. However, it is not caused by lifestyle factors or autoimmunity, and in many cases, people with MODY do not require insulin therapy right away.
Treatment varies depending on the specific gene affected, but MODY is often managed with oral medications such as glibenclamide or metformin, both of which help regulate blood sugar levels.
In some cases, if the condition progresses or blood glucose becomes difficult to control, insulin injections may be prescribed. Accurate genetic testing and diagnosis are key to ensuring proper treatment and avoiding misclassification with other diabetes types.
- Latent Autoimmune Diabetes in Adults (LADA)
Latent autoimmune diabetes in adults (LADA) is a form of autoimmune diabetes that specifically affects adults, and it represents a hybrid between Type 1 and Type 2 diabetes. Although it is often initially misdiagnosed as Type 2 due to the age of onset, LADA shares the same autoimmune origins as Type 1 diabetes, where the body’s immune system gradually destroys the insulin-producing beta cells in the pancreas.
This type is particularly suspected in adults who are initially thought to have Type 2 diabetes but who rapidly lose pancreatic function and require insulin therapy much earlier than expected. LADA typically progresses more slowly than Type 1, which can make early diagnosis challenging.
As one of the 8 types of diabetes, LADA emphasizes the need for careful medical assessment to ensure appropriate treatment. Once diagnosed, individuals with LADA often start on oral diabetes medications, but due to the progressive loss of insulin production, insulin injections are usually necessary over time to maintain proper glucose control.
- Diabetes Insipidus
Diabetes insipidus is a rare and distinct condition among the 8 types of diabetes, although it differs significantly from the glucose-related types like Type 1 and Type 2. Instead of affecting blood sugar levels, diabetes insipidus involves disruption in the body’s ability to regulate water balance through the hormone known as antidiuretic hormone (ADH), also called vasopressin.
The condition occurs either due to a deficiency in ADH production by the brain (central diabetes insipidus), or because the kidneys are unable to respond appropriately to the hormone (nephrogenic diabetes insipidus).
This leads to an inability to concentrate urine, causing excessive urination (polyuria) and, consequently, severe fluid loss and dehydration. One of the hallmark symptoms is constant and extreme thirst as the body attempts to replenish lost fluids.
Treatment of diabetes insipidus depends on the underlying cause. Options may include synthetic ADH (desmopressin) for hormone replacement, or the use of diuretics, anti-inflammatory drugs, or other medications that help reduce urine output or enhance kidney sensitivity to ADH.
Despite being distinct from typical blood sugar-related diabetes, diabetes insipidus remains an important inclusion in the classification of 8 types of diabetes due to its systemic impact and similar name.
- Secondary Diabetes
Secondary diabetes refers to diabetes that arises as a direct result of another medical condition or external factor, rather than from a primary dysfunction of insulin production or use. This type is included among the 8 types of diabetes because it can closely mimic either Type 1 or Type 2 diabetes in terms of symptoms and progression.
A variety of underlying health conditions or causes can trigger secondary diabetes. These include:
- Diseases affecting the pancreas, such as pancreatic tumors, chronic pancreatitis, pancreatic infections, or cystic fibrosis, which can damage the organ’s insulin-producing cells.
- Hormonal disorders like Cushing’s disease, pheochromocytoma, or acromegaly, which interfere with normal metabolic functions and glucose regulation.
- Medication-induced diabetes, especially due to prolonged use of drugs like corticosteroids, which are known to affect glucose metabolism.
Management of secondary diabetes primarily involves addressing the root cause—whether it’s through surgery, medication adjustment, or treatment of the hormonal disorder. At the same time, doctors may recommend oral antidiabetic medications or insulin therapy to manage blood sugar levels, depending on how severely the secondary condition affects glucose balance.
Confirming a Diagnosis
The process of confirming a diagnosis for any of the 8 types of diabetes typically begins with a thorough evaluation conducted by a qualified endocrinologist or primary care provider.
This assessment involves taking a detailed look at the patient’s symptoms, the timeline of symptom onset, family medical history, and any relevant lifestyle factors that might contribute to or explain blood sugar abnormalities or hormonal imbalances.
To accurately identify which of the 8 types of diabetes a person may have, healthcare professionals rely on a variety of diagnostic laboratory tests. Commonly ordered tests include:
- Fasting blood glucose test, which measures blood sugar levels after a period of not eating
- Hemoglobin A1c test, which reflects average blood glucose levels over the past two to three months
- Oral glucose tolerance test (OGTT), which evaluates how efficiently the body processes sugar over a few hours
These tests are essential tools to distinguish between Type 1, Type 2, gestational diabetes, and some other less common types like LADA and MODY.
When diabetes insipidus is suspected—one of the more distinct types among the 8 types of diabetes—additional specialized testing may be required. These may include a 24-hour urine collection to assess total urine output and concentration, or a water deprivation test, which helps determine the body’s ability to concentrate urine and regulate hydration through the hormone vasopressin (ADH).
Each diagnostic approach is tailored based on the suspected type of diabetes, ensuring that treatment plans are accurately matched to the patient’s individual needs and underlying condition.
Conclusion
Understanding and correctly diagnosing the 8 types of diabetes is crucial for effective treatment and long-term management. While Type 1 and Type 2 diabetes are the most commonly known, other forms like gestational diabetes, LADA, MODY, diabetes insipidus, and secondary diabetes also require tailored care.
Each type presents with different challenges and implications for health, but the key to managing them lies in early detection, informed medical guidance, and ongoing monitoring. With the right diagnosis—supported by appropriate testing and professional evaluation—individuals can take control of their condition and significantly improve their quality of life.
As research continues to evolve, awareness of the 8 types of diabetes will help more people receive timely and accurate treatment. Whether the condition is temporary, inherited, autoimmune, or secondary to another illness, the road to better health begins with understanding the type of diabetes you have and following a personalized care plan.

A graduate of Computer Science and Information Management Technology. Diploma – Caregiving, Certificates – Dementia and Diabetes Awareness and Management. A researcher, blogger, songwriter, singer and acoustic guitarist. Born in an environment where natural talents such as healing are imparted at our natural birth. This natural talents of healing is the result of our genetic inheritance and the training from family environment.