Yeast Infection Treatments: Vaginal, Oral, Skin, and More
Yeast Infection Treatments: Vaginal, Oral, Skin, and More: Yeast infections, medically referred to as candidiasis, are commonly addressed through antifungal medications tailored to the location and severity of the infection.
Yeast Infection Treatments may involve oral tablets, topical creams, or vaginal suppositories, depending on the area of the body impacted. These treatments are typically effective when applied correctly, and the specific approach often varies based on whether the infection is vaginal, cutaneous (skin), oral, or intestinal.
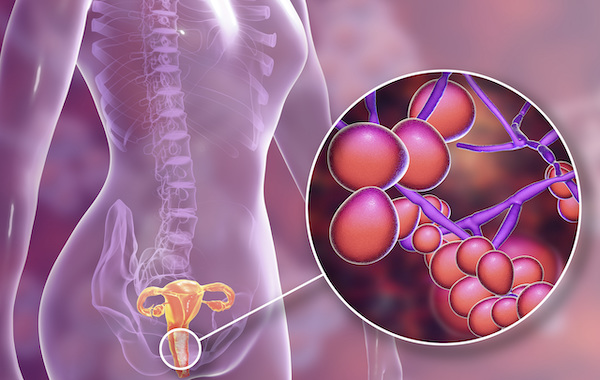
Candidiasis is caused by an overgrowth of Candida albicans, a fungal organism naturally present in the human body. While small amounts of this fungus exist harmlessly in the mouth, gastrointestinal tract, genital area, and on the skin, various factors can trigger its excessive growth.
When this imbalance occurs, clinical symptoms begin to appear, requiring appropriate Yeast Infection Treatments to restore balance and alleviate discomfort.
Yeast infections can develop in individuals regardless of age or gender, although some forms are more common in certain populations. For example, vaginal yeast infections are particularly prevalent among women, while oral thrush can affect both infants and adults with weakened immune systems.
Skin-based yeast infections, on the other hand, often appear in warm, moist areas of the body, such as under the breasts, in the groin, or between skin folds. Identifying the exact location of the infection is crucial for selecting the right form of Yeast Infection Treatments.
Causes and Risk Factors of Yeast Infections
The human body naturally maintains a balanced internal environment where beneficial bacteria and fungi coexist. However, when this balance is disturbed—whether through illness, medications like antibiotics or corticosteroids, poor hygiene, high blood sugar levels, or compromised immunity—Candida albicans can multiply unchecked.
This overgrowth leads to the development of a yeast infection, which must then be treated with suitable Yeast Infection Treatments based on the infection’s location and severity.
Hormonal fluctuations, such as those occurring during pregnancy, menstruation, or while taking birth control pills, may also increase the likelihood of a yeast infection.
Similarly, individuals with diabetes are at higher risk due to elevated blood sugar levels that create an environment conducive to fungal growth.
Recognizing these risk factors helps in the prevention and early intervention of infections using the right Yeast Infection Treatments.
Symptoms and Areas Affected by Yeast Infections
The symptoms of a yeast infection vary significantly depending on the area of the body that is affected. In vaginal infections, women often report itching, irritation, and a thick, cottage cheese-like discharge.
Burning sensations during urination or intercourse are also common. In such cases, Yeast Infection Treatments usually involve antifungal creams or vaginal suppositories, which help eliminate the fungus and restore natural flora.
Oral yeast infections, commonly called oral thrush, present differently. They are characterized by creamy white patches on the tongue, inner cheeks, and sometimes on the roof of the mouth or throat.
Pain, redness, and difficulty swallowing may also be experienced. Oral Yeast Infection Treatments typically include antifungal mouth rinses or systemic medications that treat the infection from within.
When the skin is involved, yeast infections—also known as cutaneous candidiasis or mycosis—appear as red, inflamed rashes that may itch or produce white, raised lesions. These infections often occur in areas where moisture is trapped.
Types of Yeast Infection Treatments
The choice of treatment for yeast infections largely depends on the location and severity of the infection. Since candidiasis can affect different parts of the body, Yeast Infection Treatments must be tailored to the specific area involved. Whether the infection is vaginal, oral, cutaneous, or systemic, effective management relies on the correct form and duration of therapy.
- Vaginal Yeast Infection
Among the most common types of candidiasis, vaginal yeast infections require targeted medical care. It is highly recommended that women experiencing symptoms consult with a healthcare provider or gynecologist to receive a proper diagnosis and appropriate Yeast Infection Treatments. The therapeutic options available include topical, vaginal, and oral antifungal medications.
- Topical Vaginal Creams: These antifungal creams, such as terconazole, tioconazole, or nystatin, are typically applied once daily either to the external vaginal area or inserted into the vaginal canal. Application is preferably done at night, allowing the medication to work while the body is at rest. Many of these creams are supplied with an applicator to ensure proper and hygienic use. As part of standard Yeast Infection Treatments, these topical options can offer fast relief from itching, irritation, and discharge.
- Vaginal Tablets (Suppositories): Another effective method includes the use of vaginal tablets like miconazole, isoconazole, or terconazole. These antifungal suppositories are inserted into the vagina using either a clean finger or the applicator that usually accompanies the product. As with creams, they are best used at bedtime to allow the medication to remain in place for optimal absorption and effectiveness. These forms of Yeast Infection Treatments are especially convenient for those who prefer localized treatment with minimal systemic effects.
- Oral Antifungal Pills: In cases where topical or vaginal treatments are not sufficient or preferred, oral antifungal medications such as fluconazole (typically in 150 mg dosage) or ketoconazole (200–400 mg) may be prescribed. These are usually taken as a single dose or over a short course, depending on the doctor’s recommendation. Oral Yeast Infection Treatments offer the advantage of convenience and are often used when infections are recurrent or particularly persistent.
The duration of treatment for vaginal yeast infections can vary significantly. It may last anywhere from a single day to as long as two weeks, depending on the type of medication used and the severity of the infection.
Regardless of the duration, it is crucial to complete the full course of the prescribed Yeast Infection Treatments to ensure complete eradication of the fungus and to prevent recurrence. Skipping doses or ending treatment prematurely may allow the infection to return or become resistant to medication in the future.
- Yeast Infections in Men
Although yeast infections are more commonly associated with women, men can also experience candidiasis, particularly in the genital area, including the penis, scrotum, and surrounding skin. These infections typically result from fungal overgrowth, often due to poor hygiene, compromised immunity, or after antibiotic use.
When it comes to Yeast Infection Treatments for men, proper medical evaluation is crucial. A urologist should be consulted to confirm the diagnosis and guide treatment effectively.
The standard course of treatment for yeast infections in men includes antifungal medications such as clotrimazole, miconazole, or nystatin. These are usually prescribed in the form of topical creams or oral tablets, depending on the severity and spread of the infection.
In most cases, the topical cream is applied directly to the affected genital area two to three times a day. The treatment period often lasts up to three weeks, even if symptoms such as redness, itching, or irritation begin to subside earlier. Continuing the full course of Yeast Infection Treatments helps ensure that the fungal overgrowth is completely eliminated and prevents recurrence.
In some cases, especially when symptoms are more severe or persistent, a single oral dose of fluconazole may be prescribed. This systemic antifungal medication works from within the body and can be particularly useful in treating yeast infections that are not limited to surface skin.
While Yeast Infection Treatments for men are generally straightforward, early diagnosis and adherence to medical advice are essential for fast and complete recovery.
- Yeast Infections During Pregnancy
Yeast infections are especially common during pregnancy, largely due to the natural hormonal changes and immune system alterations that occur during this time. Pregnant women often experience increased vaginal discharge and changes in vaginal pH, both of which can create an environment conducive to fungal growth.
Therefore, it is not uncommon for expectant mothers to require Yeast Infection Treatments during any trimester of pregnancy.
Treatment of yeast infections in pregnant women should always be supervised by a qualified obstetrician. The safety of both mother and baby is a priority, and as such, certain medications and delivery methods are preferred.
A commonly recommended option for Yeast Infection Treatments during pregnancy is the use of clotrimazole vaginal suppositories. These are considered safe for both the mother and developing fetus and are typically effective in resolving symptoms.
The vaginal suppository is inserted using an applicator, which helps to place the medication deep enough into the vaginal canal for optimal results while minimizing the risk of irritating or damaging the cervix.
Treatment duration may vary, but it often extends over several days to ensure the complete removal of the fungal overgrowth.
It is especially important to complete Yeast Infection Treatments before childbirth. If left untreated, the infection can potentially be transmitted to the baby during delivery, leading to complications such as oral thrush in the newborn.
Ensuring proper treatment also helps alleviate the discomfort and prevent complications like preterm labor triggered by infections. For these reasons, any symptoms of a yeast infection during pregnancy should be promptly discussed with a healthcare provider to determine the most suitable and safe treatment approach.
- Intestinal Yeast Infections
Candidiasis can also affect the gastrointestinal tract, particularly in individuals with weakened immunity, prolonged antibiotic use, or underlying health conditions such as diabetes. Intestinal fungal infections, though less commonly diagnosed, can cause symptoms like bloating, gas, abdominal discomfort, diarrhea, and fatigue.
When these signs are present, especially in people with risk factors, a gastroenterologist should be consulted to confirm the diagnosis and initiate appropriate Yeast Infection Treatments.
The primary medical approach for treating intestinal yeast infections typically involves a single 150 mg dose of oral fluconazole. This antifungal medication helps to suppress the overgrowth of Candida albicans within the digestive system and restore microbial balance.
However, it is essential that such treatment be carried out under the guidance of a qualified gastroenterologist, as improper use of antifungals can lead to resistance or incomplete eradication of the fungus.
In addition to antifungal medication, Yeast Infection Treatments for the intestines often include the use of supportive supplements. Probiotics containing strains such as Lactobacillus or Saccharomyces boulardii are frequently recommended.
These beneficial microorganisms help restore the natural balance of gut flora, inhibit fungal growth, and boost the body’s immune defenses. Incorporating probiotics into the treatment plan enhances gut health and may reduce the likelihood of future fungal overgrowth.
Maintaining a healthy diet, rich in fiber and low in refined sugars and processed foods, can also play a critical role in improving outcomes from intestinal yeast infections. Since sugar fuels fungal growth, reducing its intake supports the effectiveness of Yeast Infection Treatments and promotes long-term digestive health.
- Recurrent or Chronic Yeast Infections
When yeast infections occur multiple times within a short period, they are classified as recurrent or chronic. This condition can be both physically uncomfortable and emotionally frustrating. Recurrent infections may indicate an underlying issue that has yet to be addressed, which is why a thorough medical evaluation is essential.
A key goal in managing chronic cases is to not only treat the current infection but also prevent future episodes through targeted Yeast Infection Treatments and lifestyle modifications.
Recurrent yeast infections can arise due to various factors. These include frequent use of antibiotics, hormonal fluctuations linked to birth control or pregnancy, weakened immune function, underlying illnesses, and even external factors like wearing synthetic or tight-fitting clothing that traps moisture. Identifying the specific cause behind these repeated infections is a crucial step toward long-term resolution.
Once the underlying triggers have been recognized, adjustments can be made to minimize the risk of recurrence. These may involve changes in personal hygiene practices, dietary improvements, and environmental modifications.
In many cases, doctors may recommend a long-term management plan involving probiotics and a daily low-dose antifungal medication. This approach helps to keep fungal populations under control and prevents flare-ups.
Another important aspect of Yeast Infection Treatments for chronic infections is immune support. Strengthening the immune system through proper nutrition, stress management, adequate sleep, and regular physical activity can greatly reduce the susceptibility to future infections.
In individuals taking antibiotics, it’s especially important to supplement with probiotics, as these medications tend to disrupt the natural microbial balance that protects against fungal overgrowth.
By combining antifungal medications, probiotic support, and lifestyle interventions, recurrent yeast infections can be managed effectively and, in many cases, completely prevented. Ensuring adherence to the full treatment regimen and addressing root causes makes this holistic approach to Yeast Infection Treatments the most sustainable over time.
- Oral Thrush
Oral thrush, which is the term commonly used to describe a yeast infection in the mouth, is caused by the overgrowth of Candida albicans in the oral cavity. This condition presents with white, creamy lesions that may appear on the tongue, inner cheeks, gums, tonsils, or even the back of the throat.
It can cause discomfort, difficulty swallowing, and in some cases, changes in taste. For proper management, oral thrush should be evaluated and treated by a gastroenterologist or another qualified healthcare provider to ensure that the correct form of Yeast Infection Treatments is administered.
Treatment for oral thrush typically involves antifungal medications that are either used topically within the mouth or taken systemically. A commonly prescribed topical treatment is an oral antifungal solution, such as nystatin, which is swished thoroughly around the mouth and then swallowed to ensure that both superficial and deeper areas are reached.
For more persistent or widespread infections, oral antifungal pills such as fluconazole may be prescribed in a single or multi-dose regimen. These medications are part of a standard set of Yeast Infection Treatments designed to control fungal overgrowth in the oral mucosa and prevent its spread.
Maintaining proper oral hygiene during treatment is also essential for recovery. Brushing the teeth at least three times daily and using a soft-bristled toothbrush can help prevent the fungus from re-accumulating on oral surfaces.
Rinsing the mouth with a saltwater solution or a mild antiseptic can further reduce microbial load and assist in the healing process. Following medical advice closely and maintaining oral cleanliness helps maximize the effectiveness of Yeast Infection Treatments for oral thrush.
Home Remedies for Yeast Infections
In addition to pharmaceutical interventions, some individuals explore natural or home-based options to complement their prescribed Yeast Infection Treatments. One widely recognized home remedy is the use of plain, unsweetened natural yogurt.
Yogurt contains live probiotic cultures, particularly Lactobacillus, which can help maintain or restore the natural microbial balance in the body and inhibit the growth of Candida albicans.
For vaginal yeast infections, applying yogurt directly can support recovery by regulating vaginal pH and creating an environment that discourages fungal growth. This method involves soaking a clean tampon in natural yogurt and inserting it into the vagina, allowing it to remain in place for at least three hours.
This approach, while not a substitute for clinical treatment, is often used to complement medical Yeast Infection Treatments, especially in mild cases or as preventive care.
Men experiencing genital yeast infections can also benefit from applying natural yogurt directly to the affected area, especially to the tip of the penis. The cooling and anti-inflammatory properties of yogurt may help reduce itching, redness, and irritation.
As part of a holistic plan, these natural remedies may support the body’s healing process when used alongside doctor-approved Yeast Infection Treatments.
It is important to note that while home remedies like yogurt may offer some relief, they should not replace medical advice or prescribed antifungal medications.
For individuals with frequent or severe infections, professional guidance is necessary to ensure that Yeast Infection Treatments are appropriately tailored and effective. Combining traditional treatment methods with supportive lifestyle changes and natural remedies can often lead to better outcomes and reduced risk of recurrence.
Additional Considerations During Yeast Infection Treatments
When undergoing Yeast Infection Treatments, several supportive measures can help enhance effectiveness and reduce the likelihood of recurrence. These additional considerations, although sometimes overlooked, are valuable for both managing current infections and preventing future ones.
Maintaining excellent personal hygiene is essential. Individuals—regardless of gender—should focus on keeping the affected area, especially the genital region, clean and dry. Fungal organisms thrive in moist environments, so minimizing moisture helps to slow or stop the spread of infection.
This becomes even more important when applying topical Yeast Infection Treatments, as dry skin and fabric contact ensure the medication stays effective longer.
Wearing breathable, loose-fitting clothing made from cotton or other natural fibers can also help reduce fungal overgrowth. Tight or synthetic fabrics may trap heat and sweat, creating the perfect environment for Candida to multiply. Making this simple switch can improve comfort and support the action of prescribed Yeast Infection Treatments.
Using condoms during sexual contact is another important precaution. Sexual activity can sometimes exacerbate symptoms or cause reinfection, especially if a partner is unknowingly carrying the fungus. Condoms can help reduce transmission and protect both partners while undergoing Yeast Infection Treatments.
Limiting unnecessary medications—particularly antibiotics—is also essential. Antibiotics can disrupt the body’s natural microbial balance by killing beneficial bacteria that normally keep fungal populations in check.
If antibiotics are needed for other health issues, consider taking probiotics at the same time, as this can help maintain microbial equilibrium and improve the success of concurrent Yeast Infection Treatments.
A well-balanced diet plays a key role, too. Drinking plenty of water helps flush out toxins and keeps the body hydrated, which is beneficial during recovery. Consuming more greens, vegetables, and fresh fruits helps to support immune function, while cutting down on processed foods, fatty meals, sugary snacks, and alcohol can minimize conditions that encourage fungal growth.
This dietary strategy aligns closely with the principles of the Candida diet, which is designed to complement Yeast Infection Treatments and prevent future infections.
These lifestyle habits are recommended for both men and women, regardless of age, and serve as practical, everyday tools for supporting the effects of medical Yeast Infection Treatments.
Signs That Yeast Infection Treatments Are Working
Recognizing when a yeast infection is improving is reassuring and can help individuals remain consistent with their treatment regimen. In cases of vaginal yeast infections, improvement is usually marked by a noticeable reduction in itching, burning, and redness.
The thick, white vaginal discharge associated with infection may also decrease significantly in volume and consistency. These are all clear indicators that Yeast Infection Treatments are beginning to work and that the infection is responding to medication.
For intestinal yeast infections, positive changes might include more regular bowel movements, a decrease in gas and bloating, and an overall increase in energy levels and vitality. Patients often report feeling stronger and more comfortable as their digestive system begins to normalize, signaling that the prescribed Yeast Infection Treatments are effectively controlling the fungal overgrowth.
Signs That the Infection May Be Worsening
While many yeast infections resolve with proper care, it’s also important to know when to seek urgent medical attention. If symptoms become more severe or do not improve with treatment, it could indicate a resistant infection or a deeper underlying issue.
Warning signs that a yeast infection is worsening may include persistent or escalating nausea and vomiting, severe abdominal or pelvic pain, high fever accompanied by chills, or prolonged loss of appetite. These symptoms may point to a systemic fungal infection or complications from untreated candidiasis. In such cases, relying solely on standard Yeast Infection Treatments may not be sufficient.
If any of these signs are present, it is critical to go to a hospital or consult a physician immediately. Advanced care or a different course of antifungal therapy may be necessary to prevent serious health consequences.
Early intervention not only ensures a better prognosis but also prevents further complications associated with ineffective or incomplete Yeast Infection Treatments.

A graduate of Computer Science and Information Management Technology. Diploma – Caregiving, Certificates – Dementia and Diabetes Awareness and Management. A researcher, blogger, songwriter, singer and acoustic guitarist. Born in an environment where natural talents such as healing are imparted at our natural birth. This natural talents of healing is the result of our genetic inheritance and the training from family environment.