Novel mRNA Cancer Vaccine Enhances Immune Response Against Fatal Brain Tumors – Glioblastoma, the predominant form of brain cancer, affects approximately 3 out of every 100,000 individuals worldwide annually.
Recent studies indicate a rising incidence of glioblastoma, attributed to factors like an aging populace and environmental elements such as air pollution.
With an average five-year survival rate of 6.9%, glioblastoma poses significant treatment challenges. However, researchers at the University of Florida have pioneered a groundbreaking mRNA cancer vaccine designed to stimulate the immune system’s response against glioblastoma.
Published in the journal Cell, their findings offer promising insights into potential treatment avenues for this formidable disease.
Dr. Elias Sayour, the Stop Children’s Cancer/Bonnie R. Freeman Professor for Pediatric Oncology Research at the University of Florida, and the lead author of the study, emphasized the persistent lack of substantial advancements in glioblastoma treatment despite medical innovations.
He highlighted the university’s brain tumor program’s exploration of various immunotherapy approaches and the development of a novel mRNA vaccine to augment responses against these challenging malignancies.
Advancements in Personalized mRNA Cancer Vaccines
Following the success of mRNA vaccines in combating the coronavirus, researchers have turned their attention to exploring their potential in treating other diseases, particularly cancer.
In a groundbreaking study, scientists utilized patients’ own tumor cells to develop tailored vaccines specific to their individual cancer types.
Dr. Elias Sayour, leading the research, elucidated, “mRNA serves as the blueprint from our genetic makeup, shaping the distinct protein profiles defining both individuals and cancers.”
He further explained, “By targeting the unique mRNA signatures of each patient’s cancer, we can craft highly personalized vaccines tailored to individual tumors, offering a scalable solution applicable across diverse cases.”
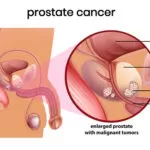
SEE ALSO:Symptoms and Signs of Prostrate Cancer
Efficacy of mRNA Vaccine in Eliciting Immune Response
The study assessed the efficacy of these innovative mRNA vaccines through trials involving ten pet dogs diagnosed with natural brain tumors, recruited when conventional treatment options were exhausted.
Remarkably, dogs treated with the mRNA cancer vaccine exhibited a substantial improvement, with an average survival period of 139 days, a stark contrast to the typical survival window of merely 30 to 60 days.
Building upon successful animal trials, the researchers expanded their investigation to include a small FDA-approved clinical trial involving four human participants diagnosed with glioblastoma.
Following administration of the mRNA vaccine, researchers observed a rapid transition in less than 48 hours, from a dormant “cold” immune response to an active “hot” immune response against brain tumors.
Dr. Sayour highlighted the significance of this swift immune activation, stating, “Typically, vaccines require weeks to months, along with booster doses, to initiate a response. Our findings suggest a paradigm shift, enabling swift immune system activation against cancer.”
He emphasized the potential impact of this approach in empowering the immune system to combat rapidly evolving tumors, providing it with a vital head start in the battle against cancer.
Further Validation Through Expanded Clinical Trials
While the clinical impact of the mRNA cancer vaccine is yet to be fully understood, scientists have noted encouraging outcomes among human study participants. These individuals either experienced extended disease-free periods or surpassed anticipated survival rates.
The researchers emphasized the importance of conducting larger clinical trials to confirm these initial findings. The small-scale trial involving four participants provided valuable insights into the vaccine’s safety and feasibility, laying the groundwork for expanded research endeavors.
Dr. Sayour underscored the necessity of validating these results through broader patient cohorts, determining optimal dosage levels, and advancing to phase II trials. Additionally, efforts are underway to extend this innovative approach to combat pediatric brain tumors, further expanding its potential impact in oncology.
Further Investigation Required for Cancer Vaccines Targeting Glioblastoma
Dr. Wael Harb, a board-certified hematologist and medical oncologist at MemorialCare Cancer Institute, highlighted the pressing need for innovative treatments for glioblastoma, considering its formidable treatment challenges.
Dr. Harb, not involved in the study, expressed optimism regarding the study’s approach, emphasizing the potential of leveraging systemic immune responses to reprogram the tumor microenvironment.
“The overall strategy is very interesting using the systemic immune response while reprogramming the tumor microenvironment is very promising — and in the larger context of immunotherapy research, I think this is a really exciting approach,” Dr. Harb commented.
He stressed the importance of advancing to well-designed clinical trials to assess the safety and efficacy of RNA-LPAs (RNA lipid-particle aggregates) in reprogramming the tumor microenvironment. Dr. Harb emphasized the significance of incorporating biomarkers to validate the mechanism of action.
YOU MAY LIKE:Best Diet for Cancer Prevention
“To me, this is a way of educating the immune cells [on] how to fight cancer,” Dr. Harb continued.
He emphasized the need to closely monitor the outcomes of early-phase clinical trials to evaluate safety, efficacy, and biomarker correlations between human and animal studies.
Dr. Jose Carrillo, a board-certified neurologist and neuro-oncologist at Pacific Neuroscience Institute, echoed Dr. Harb’s sentiments, expressing cautious optimism in response to the study’s findings.
“This study describes a novel technique for inducing an immune response in glioblastoma, which has been notoriously difficult to obtain significant advances in survival with immune therapies and clinical trials,” Dr. Carrillo noted.
He remained hopeful that continued research efforts, like the one described in the study, would contribute to unraveling new treatment avenues for glioblastoma, ultimately improving outcomes for patients.
Source: medicalnewstoday.com

A graduate of Computer Science and Information Management Technology. Diploma – Caregiving, Certificates – Dementia and Diabetes Awareness and Management. A researcher, blogger, songwriter, singer and acoustic guitarist. Born in an environment where natural talents such as healing are imparted at our natural birth. This natural talents of healing is the result of our genetic inheritance and the training from family environment.