Facts on Heart Failure Symptoms
Heart failure happens when the heart doesn’t pump blood as well as it should. The resultant effect creates several heart failure symptoms. This can lead to a backup of blood and fluid buildup in the lungs, which can make it hard to breathe.
Some heart problems gradually weaken or stiffen the heart, making it difficult for it to fill and pump blood properly. These problems can include narrowed arteries in the heart and high blood pressure.
Treatment for heart failure can help improve symptoms and might even help people live longer. Making changes in lifestyle, like losing weight, exercising, reducing salt intake, and managing stress, can also make a big difference in how you feel.
However, heart failure can be very serious and even life-threatening. Some people with heart failure have severe symptoms, and in some cases, they might need a heart transplant or a device to help their heart pump blood.
Heart failure is sometimes also called congestive heart failure. It’s important to take it seriously and work closely with doctors to manage it.
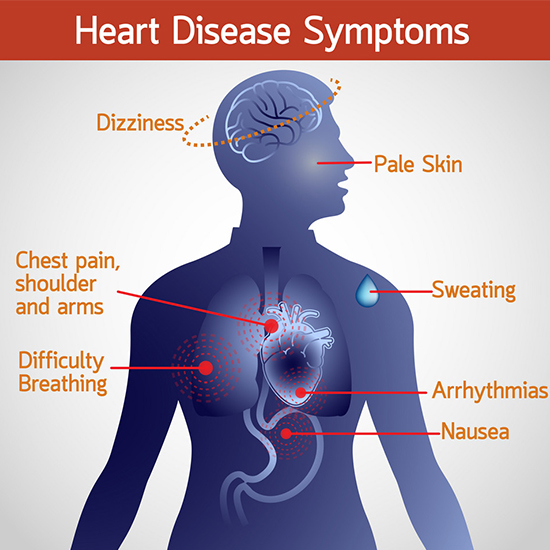
Heart Failure Symptoms
When you have heart failure, your heart can’t pump enough blood to keep up with what your body needs.
Symptoms of heart failure can show up slowly over time, or they might come on suddenly. These symptoms can include:
- Feeling short of breath when you’re active or lying down.
- Feeling tired and weak.
- Swelling in your legs, ankles, and feet.
- Having a fast or irregular heartbeat.
- Finding it harder to exercise like you used to.
- Making wheezing sounds when you breathe.
- Having a cough that sticks around or brings up white or pink mucus with a little blood.
- Swelling in your belly area.
- Quickly gaining weight because of fluid buildup.
- Feeling sick to your stomach and not wanting to eat.
- Having trouble focusing or feeling less alert.
- Feeling chest pain if your heart failure was caused by a heart attack.
These symptoms can vary from person to person, and not everyone with heart failure will have all of them. If you notice any of these signs, it’s important to talk to your doctor right away.
Let’s dive deeper
Recognizing the Warning Signs Early
Heart failure is a chronic condition that weakens the heart’s ability to pump blood effectively throughout the body. This can lead to a buildup of fluid in the lungs and other organs, causing various symptoms that can significantly impact a person’s quality of life. Early detection and treatment of heart failure are crucial for managing the condition and improving long-term health outcomes.
This blog post aims to empower you with knowledge about the common symptoms of heart failure. By recognizing these warning signs early, you can seek prompt medical attention and work with your doctor to manage the condition effectively.
Heart Failure Symptoms:
- Shortness of Breath (Dyspnea): One of the most frequent symptoms of heart failure is shortness of breath, often described as a feeling of air hunger. This breathlessness typically worsens with physical activity or while lying down at night due to fluid accumulation in the lungs.
- Fatigue and Weakness: People with heart failure often experience excessive tiredness and weakness, even during minimal activities. This extreme fatigue can make it difficult to carry out daily tasks and significantly reduce your quality of life.
- Swelling in Ankles, Legs, and Feet (Edema): Fluid buildup due to heart failure can cause swelling, particularly in the lower extremities like the ankles, legs, and feet. This swelling may worsen throughout the day and improve slightly with elevation.
- Rapid or Irregular Heartbeat (Palpitations): A racing or irregular heartbeat, medically known as palpitations, can be a symptom of heart failure. You might feel like your heart is fluttering, pounding, or skipping beats.
- Persistent Cough: A chronic cough that doesn’t go away, especially worse at night when lying down, can be a sign of fluid buildup in the lungs caused by heart failure. This cough may be dry or productive, bringing up white or pink mucus.
- Reduced Appetite and Nausea: Fluid accumulation in the abdomen, a common occurrence in heart failure, can lead to a feeling of fullness and lack of appetite. You might also experience nausea, which can further decrease your desire to eat.
- Sudden Weight Gain: Rapid weight gain that can’t be explained by increased food intake can be a sign of fluid retention, a symptom of heart failure. This weight gain usually happens within a short period, like a few days or weeks.
When to Seek Medical Attention:
It’s crucial to seek immediate medical attention if you experience any combination of these symptoms, especially if they appear suddenly or worsen over time. Early diagnosis and treatment of heart failure can significantly improve your prognosis and quality of life.
SEE ALSO: Causes of High Cholesterol
Additional Information:
Several factors can increase your risk of developing heart failure, including high blood pressure, coronary artery disease, diabetes, and a family history of heart failure.
Diagnosing heart failure usually involves a combination of a physical exam, reviewing your medical history, and undergoing various tests such as chest X-rays, echocardiograms, and blood tests. Treatment options for heart failure typically involve a combination of medications, lifestyle changes (diet and exercise), and sometimes surgery.
Causes of Heart Failure
The Troubled Pump: Why Hearts Fail
Heart failure isn’t a single disease, but rather a condition where the heart struggles to keep up with its job of pumping blood throughout the body. This can happen for several reasons, affecting either the strength or the flexibility of the heart muscle.
A Weakened Pump:
Imagine your heart as a muscular pump. If the heart muscle itself becomes weak or damaged, the heart chambers might stretch and enlarge. This weakens the pump’s ability to push blood out effectively.
A Stiff Pump:
Sometimes, the problem isn’t strength, but flexibility. If the main pumping chambers (ventricles) become stiff, they can’t fill up properly with blood between beats. This again reduces the heart’s overall pumping efficiency.
Causes of Heart Muscle Damage:
- Infections: Certain infections, like those caused by viruses including COVID-19, can damage the heart muscle.
- Unhealthy Habits: Heavy alcohol and illegal drug use can also weaken the heart. Some chemotherapy medications may have similar side effects.
- Genetics: In some cases, genes play a role in heart muscle weakness.
Conditions that Strain the Heart:
These conditions put extra stress on the heart, eventually leading to weakness or stiffness:
- Coronary Artery Disease and Heart Attack: Blocked arteries starve the heart muscle of oxygen, leading to damage and weakened pumping.
- High Blood Pressure: Over time, constantly working against high blood pressure can make the heart muscle overworked and eventually weak.
- Heart Valve Disease: Leaky or blocked heart valves force the heart to work harder to pump blood, leading to potential weakening over time.
- Congenital Heart Defects: If you’re born with a heart defect, your heart may have to work extra hard to compensate, increasing the risk of failure later in life.
- Irregular Heartbeats (Arrhythmias): Both very fast or very slow heartbeats can strain the heart and contribute to failure.
Other Risk Factors:
Certain long-term health issues can also increase the risk of heart failure, such as diabetes, HIV infection, thyroid problems, and iron or protein buildup in the body.
Sudden Heart Failure Triggers:
In some cases, heart failure can develop rapidly due to:
- Severe allergic reactions
- Systemic illnesses
- Blood clots in the lungs
- Serious infections
- Certain medications
- Viruses attacking the heart muscle
The domino effect often starts in the left ventricle, the heart’s main pumping chamber. However, heart failure can eventually impact the right ventricle as well, or even affect both sides simultaneously.
Types of Heart Failure
| Type of Heart Failure | Description | Source |
| Right-sided heart failure | This type affects the lower right chamber of the heart (right ventricle). Fluid backs up into the abdomen, legs, and feet, causing swelling. | American Heart Association |
| Left-sided heart failure | This type affects the lower left chamber of the heart (left ventricle). Fluid backs up into the lungs, causing shortness of breath. | American Heart Association |
| Heart failure with reduced ejection fraction (HFrEF) or Systolic heart failure | This is a subtype of left-sided heart failure. The left ventricle can’t contract (squeeze) as forcefully as it should. The weakened heart can’t pump enough blood throughout the body. | American Heart Association |
| Heart failure with preserved ejection fraction (HFpEF) or Diastolic heart failure | This is a subtype of left-sided heart failure. The left ventricle can’t relax or fill with blood completely. The heart has difficulty filling with blood between beats. | American Heart Association |
Risk Factors for Heart Failure
Heart failure risk factors can be broadly categorized into three areas: Underlying medical conditions, lifestyle habits, and individual characteristics.
Underlying Medical Conditions:
- Coronary artery disease (CAD): Narrowed arteries due to plaque buildup starve the heart muscle of oxygen, weakening it.
- Heart attack: Past heart attacks damage heart muscle, reducing pumping efficiency.
- Heart valve disease: Leaky or blocked valves force the heart to work harder, potentially leading to weakness.
- High blood pressure (hypertension): The heart constantly struggles against high pressure, potentially leading to long-term weakening.
- Irregular heartbeats (arrhythmias): Abnormal heart rhythms, especially fast ones, can strain the heart muscle.
- Congenital heart defects: Birth defects in the heart structure or function can increase the risk of failure later in life.
- Diabetes: This condition raises the risk of both high blood pressure and coronary artery disease, which can contribute to heart failure.
- Sleep apnea: Obstructive sleep apnea reduces blood oxygen levels and increases the risk of irregular heartbeats, both of which can weaken the heart.
- Viral infections: Certain viruses can directly damage the heart muscle.
Lifestyle Habits:
- Obesity: Excess weight puts extra strain on the heart, raising the risk of failure.
- Alcohol abuse: Excessive alcohol consumption can weaken the heart muscle.
- Smoking: Smoking damages blood vessels and increases the risk of both heart disease and heart failure.
Individual Characteristics:
- Age: As we age, the heart’s function naturally declines, increasing the risk of failure.
Medications (Consult your doctor before stopping any medication):
- Certain diabetes medications: Some diabetes drugs (e.g., rosiglitazone, pioglitazone) have been linked to a higher heart failure risk in some people.
- Other medications: Certain nonsteroidal anti-inflammatory drugs (NSAIDs), high blood pressure medications, medications for cancer, blood conditions, irregular heartbeats, nervous system diseases, mental health conditions, lung and urinary problems, and infections may also increase the risk of heart failure or heart problems.
Complications:
If you have heart failure, it’s important to keep up with regular health checkups, even if you start feeling better. Your doctor can examine you and run tests to make sure everything is okay and to catch any problems early.
Complications from heart failure can vary depending on things like your age, overall health, and how severe your heart disease is. They might include:
- Kidney damage or failure: Heart failure can mean less blood flow to your kidneys. If not treated, this can lead to kidney failure. Sometimes, heart failure-related kidney damage needs treatment like dialysis.
- Other heart problems: Heart failure can change the size and function of your heart, which might damage heart valves or cause irregular heartbeats.
- Liver damage: Fluid buildup from heart failure can put too much pressure on your liver, causing scarring. This can make it harder for your liver to work right.
- Sudden cardiac death: If your heart is weak, you might be at risk of suddenly dying from a dangerous irregular heartbeat.
Prevention:
One way to avoid heart failure is by treating and controlling the conditions that can cause it, like coronary artery disease, high blood pressure, diabetes, and obesity.
Some of the same things that help manage heart failure can also help prevent it. Here are some tips for a healthy heart:
- Don’t smoke.
- Stay active with plenty of exercise.
- Eat foods that are good for your heart.
- Keep your weight in a healthy range.
- Find ways to reduce and manage stress.
- Take your medicines as your doctor tells you to.
Taking care of your heart is important for staying healthy and feeling good.
Disclaimer:
This blog provides only general information and does not constitute medical advice. Please consult with a qualified healthcare professional for diagnosis and treatment recommendations specific to your individual situation.
Conclusion:
Recognizing the early warning signs of heart failure is crucial for seeking timely medical attention and managing the condition effectively. By being aware of the symptoms mentioned above and taking proactive steps towards a healthy lifestyle, you can empower yourself to take control of your heart health.
Call to Action:
Do you have any questions about heart failure symptoms? Feel free to leave a comment below, and we’ll do our best to address them! For further reading, visit this page

A graduate of Computer Science and Information Management Technology. Diploma – Caregiving, Certificates – Dementia and Diabetes Awareness and Management. A researcher, blogger, songwriter, singer and acoustic guitarist. Born in an environment where natural talents such as healing are imparted at our natural birth. This natural talents of healing is the result of our genetic inheritance and the training from family environment.